Let’s walk through what you can expect*†:
 Doctor prescribes VYNDAMAX
Doctor prescribes VYNDAMAX
Your doctor sends your VYNDAMAX prescription to a specialty pharmacy, which will ship specialty medications to your home.
![]() Watch out for a call from the specialty pharmacy!
Watch out for a call from the specialty pharmacy!
 Confirm insurance coverage
Confirm insurance coverage
- The specialty pharmacy will contact your insurance plan to confirm your coverage for VYNDAMAX, including co-payment amounts and other financial assistance options
- The specialty pharmacy will review coverage with you over the phone and can also discuss financial assistance options

 Receive VYNDAMAX
Receive VYNDAMAX
Once your insurance is approved, the specialty pharmacy will work with you to coordinate the delivery of VYNDAMAX.

 Continuing VYNDAMAX
Continuing VYNDAMAX
- Your doctor will tell you what clinical and insurance requirements are needed to continue on VYNDAMAX
- The specialty pharmacy will coordinate with you and your doctor to make sure your information is up to date
*Access to VYNDAQEL® (tafamidis meglumine) is available through each prescription pathway.
†Limits, terms, and conditions apply. Please visit myVynAssist.com for full terms and conditions of the Co-pay Savings Program.
VYNDAMAX Free Trial Program
Talk to your doctor about the VYNDAMAX Free Trial Program. New patients may be eligible to receive a 30-day supply of VYNDAMAX at no cost.
Get support along your medication journey
- With a valid prescription, you can request support from a Patient Access Coordinator (PAC)
- A PAC is a Pfizer employee who can help you understand your insurance coverage and expected out-of-pocket costs, and help navigate getting your prescribed medicine
- They can provide updates and help streamline communications
- Connect with a PAC today at 1-888-863-1177 (Mon-Fri, 9AM-5PM ET)
Get support along your medication journey
Get support along your medication journey
- With a valid prescription, you can request support from a Patient Access Coordinator (PAC)
- A PAC is a Pfizer employee who can help you understand your insurance coverage and expected out-of-pocket costs, and help navigate getting your prescribed medicine
- They can provide updates and help streamline communications
- Connect with a PAC today at 1-888-863-1177 (Mon-Fri, 9AM-5PM ET)
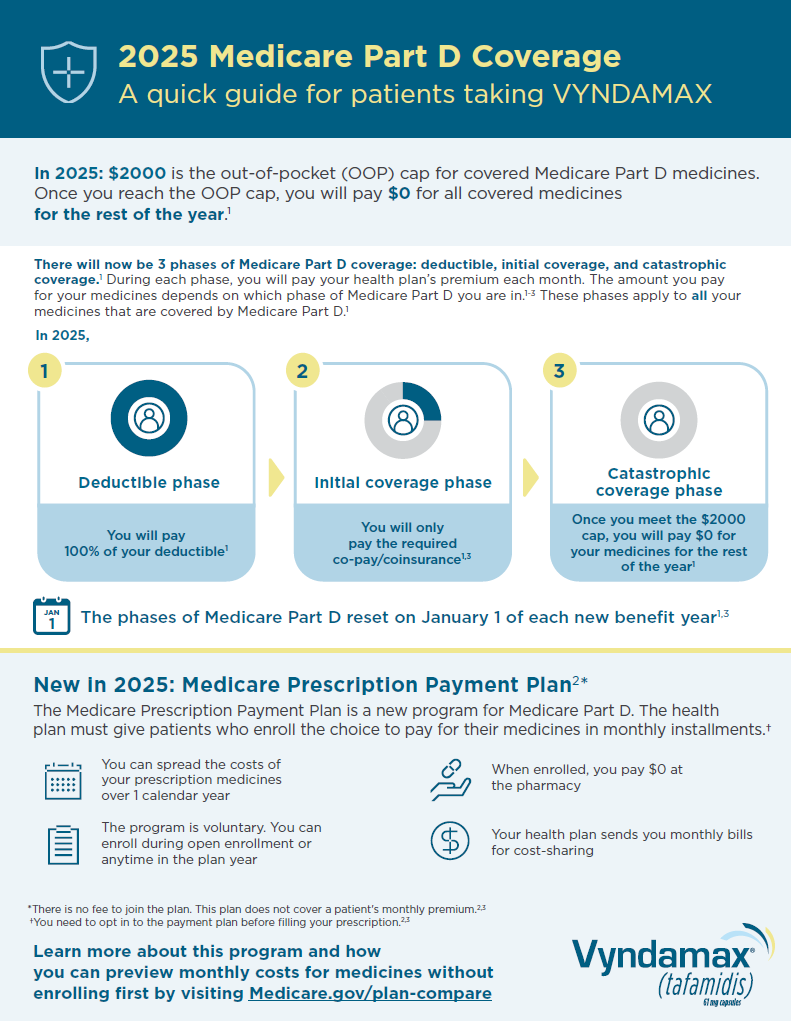
VYNDAMAX Patient Medicare Part D Flashcard
An overview of changing Medicare Part D coverage that’ll help people on Medicare better understand their out-of-pocket costs for medicines like VYNDAMAX in 2025.
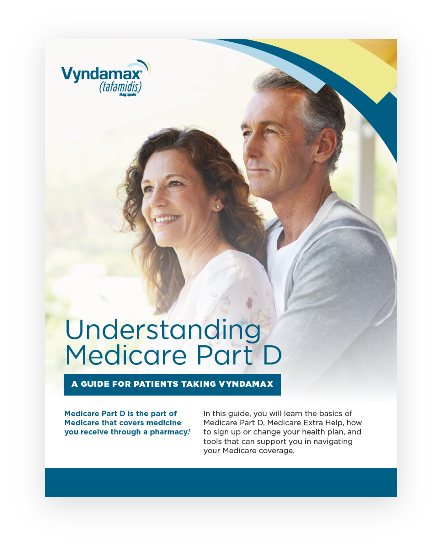
VYNDAMAX Medicare Part D Brochure
A deeper dive into the changing Medicare Part D coverage in 2025 and what to expect.
Get to the heart of what matters
Stay informed with educational materials about ATTR-CM and VYNDAMAX