Connect with a Patient Access Coordinator (PAC)
- With a valid prescription, you can request support from a PAC–your dedicated partner in navigating the VYNDAMAX access process, they'll guide you every step of the way.
Your PAC will personally:
- Help you understand your insurance coverage and benefits
- Explain what to expect when working with a specialty pharmacy
- Keep you informed with timely updates and actionable requirements
- With a valid prescription, you can request support from a PAC–your dedicated partner in navigating the VYNDAMAX access process, they'll guide you every step of the way.
Your PAC will personally:
- Help you understand your insurance coverage and benefits
- Explain what to expect when working with a specialty pharmacy
- Keep you informed with timely updates and actionable requirements
- With a valid prescription, you can request support from a PAC–your dedicated partner in navigating the VYNDAMAX access process, they'll guide you every step of the way.
Your PAC will personally:
- Help you understand your insurance coverage and benefits
- Explain what to expect when working with a specialty pharmacy
- Keep you informed with timely updates and actionable requirements
Connect with a PAC today at 1-888-863-1177 (Mon-Fri, 9AM-5PM ET)
Sometimes an insurance plan will ask for a reauthorization after some time on treatment
If that happens, you and your doctor can work together to give your insurance provider what they need, so you can continue VYNDAMAX.
Learn more about 2026 Medicare Part D changes
$2,100
is the annual out-of-pocket (OOP) cap for your covered Part D medicines. That means when you get your first VYNDAMAX prescription in 2026, you will reach the $2,100 OOP maximum. For the rest of the year, you will pay $0 for all your
Download the Medicare Part D Flashcard to learn more about what’s new in 2026
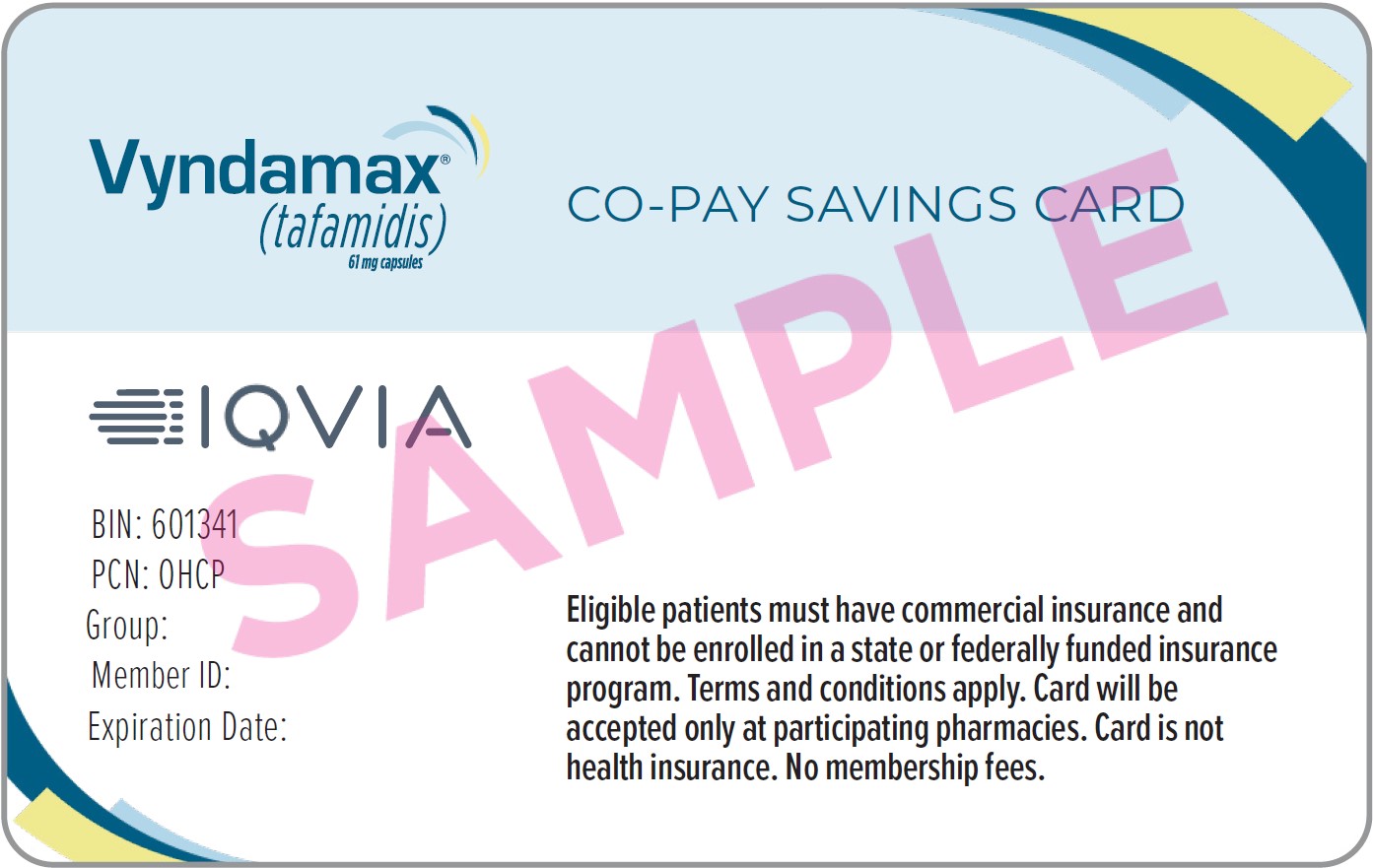
VYNDAMAX Co-pay Savings Program
Eligible, commercially insured patients may pay as little as $0 a month*
*Limits, terms, and conditions apply. Click here for full terms and conditions.
Will VYNDAQEL be available in 2026?
VYNDAMAX will be the only tafamidis option available after 2025. This decision is focused on patient convenience as VYNDAMAX offers the same active ingredient and clinical benefits as VYNDAQEL, but in just one pill once a day, making it easier for patients to take their prescription.
What do I do if I am currently taking VYNDAQEL?
If you are currently taking VYNDAQEL, talk to your healthcare provider about switching to VYNDAMAX, a more convenient dosing option for tafamidis.
A new prescription and prior authorization will likely be required to make the switch.
A Patient Access Coordinator (PAC) can help you understand the insurance approval process and answer questions about getting access to VYNDAMAX. Sign up here.
What is the difference between VYNDAQEL & VYNDAMAX?
There is no difference in how the medicines work, but VYNDAMAX offers more convenient dosing and will be the only tafamidis option available after 2025.
The difference is in how they’re taken: VYNDAMAX is one pill once a day, while VYNDAQEL requires four pills daily.
VynAssist - your home for personalized access and reimbursement support for patients prescribed VYNDAMAX.
VynAssist is here to help with your VYNDAMAX prescription by offering:
- Access support - Guide you through medication access
- Financial assistance - Connect you with potential options to help manage costs
- Support & resources - Inform you of options for personalized support and downloadable resources